Osteoporosis and gut health: how are the two linked?
With Dr Ese Stacey, Sport and Exercise Medicine Doctor

Osteoporosis and gut health: how are the two linked?
Posted on Mon Jun 10, 2019
Inflammation can increase the risk of osteoporosis. Dr Ese Stacey explains why.
Gut health and bones
Scientific research now confirms that the microbes living in our intestines play an important role in our health. A beneficial gut environment will ensure healthy digestion of food and detoxification of toxic materials. A good gut microbial balance will also help to maintain a healthy immune system and, crucially, will help to keep levels of inflammation in the body down.
Low grade chronic inflammation is known to be responsible for almost all chronic ill health. Understanding the gut and the factors that impact on gut microbes is central to understanding how to stay well or regain good health.
Inflammation and osteoporosis
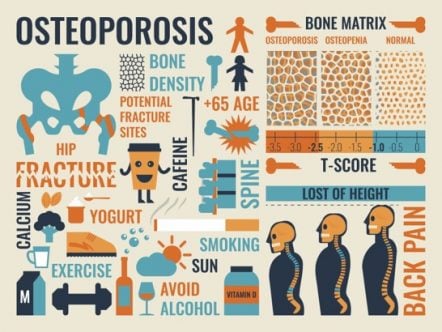
Bone is a living organ which is constantly being built up and broken down. This is called bone turnover. Good bone health requires a balance between the cells that build (osteoblasts) and the cells that breakdown (osteoclasts).
When there is a mismatch between the two and there is more bone break-down than bone building, the result is net bone loss. This can result in below average bone density which is called osteopenia. When bone density gets very low, it is called osteoporosis. With osteoporosis there is an increased risk of bone fracture.
The body views inflammation as a ‘stressful’ event, so the way it responds to this stress is to cease normal bone turnover in favour of bone loss. This means that anything that causes inflammation may have an effect on bone health.
We can look for clues for the origins of suboptimal bone health when we ask about other health issues. If we focus on the causes of inflammation, we are likely to deal with not only the osteoporosis, but with other associated conditions as well.
Infection & Immunity
Chronic infection causes chronic inflammation. Chronic infection also puts a continual added burden on the immune system. Obvious infections such as repeated tonsillitis, pneumonias, skin infections, urine or yeast infections are easily spotted. Less obvious is when chronic gut dysbiosis leads to ‘leaky gut’. The leaky gut may allow entrance to a variety of different organisms including viruses and bacteria.
When the immune system has been dealing with a situation for some time, at some stage it may become overwhelmed. This means that rather than fight the continual bombardment of infections, the immune cells responsible for defence are unable to mount a response and simply let the invading pathogens into the body.
When this situation occurs, we find that immune markers (measured on blood tests) are suppressed. With specialized testing we may also find markers of the various viruses and bacteria in the blood stream. A suppressed immune system, together with chronic infection, will give symptoms of chronic fatigue.
In dealing with the osteoporosis, it is important that we address both the suppressed immune system as well as any chronic infections. Very rarely, osteoporotic fractures of the spine can be associated with infections. These would typically occur in patients with a suppressed immune system from chronic infection or from chronic corticosteroid use. Chronic tooth infection and cavitations which may be asymptomatic, may be sources of chronic inflammation.
Toxins
Certain toxins such as cadmium and lead are known to have a negative impact on bone health. Others have a suggested link with bone loss e.g pesticides. Toxins that have a known association with gum disease are also likely to impact on general bone health.
Other toxins such as plastics or leaching mercury from old fillings may be associated with osteoporosis by virtue of causing chronic inflammation. Most toxins do not give direct symptoms and most people are unaware that they have toxin overload.
Cigarette smoke produces a compound related to cyanide (thiocynate) which has an affinity for bone. Thiocynate is also found in certain foods and other compounds and can cause low iodine levels and hence hypothyroidism.
The environment you grew up in is also very relevant to bone disease as many of the toxins will stay in the body and will not be eliminated unless specific measures are undertaken to coax them out. In order to know how to deal with the inflammation, it is important to identify which toxic chemicals are in the body. This can be done by specialized urine tests.
Vitamin deficiency and osteoporosis
Most people are aware that Vitamin D is important for good bone health. The body uses vitamins and minerals to fight inflammation. This means that after a chronic or severe fight blood levels of certain vitamins are likely to be low. The vitamins most likely to be impacted by chronic inflammation are:
- Vitamin B1
- Vitamin B2
- Vitamin B12
- Vitamin C
Vitamin C is an important component of collagen which forms bone. In certain individuals it is so low or non-existent that a diagnosis of scurvy is made. The symptoms of scurvy are fatigue, sore arms and legs, bleeding gums and skin and you guessed it, bone loss.
Vitamin K2 is little talked about in mainstream medicine however it is crucial for good bone health. It is not to be confused with vitamin K1 found in green, leafy vegetables. Vitamin K2 is fat soluble and found in liver, fermented soya (Natto) and foie gras. In Japan vitamin K2 supplementation is used as a treatment for osteoporosis.
It is difficult to measure vitamin K2 directly, however research papers suggest that most of the population is low in vitamin K2. In fact 3 out of the 4 fat soluble vitamins (A, D, and K) are likely to be required for good bone health. Vitamin A and D are responsible for the absorption of calcium from the intestine. Vitamin K2 is then required to ensure that the calcium is integrated into bone.
Holistic support for osteopenia and osteoporosis
Identifying the main factors that cause inflammation is the first step to supporting the body back to equilibrium. My approach to recovery is to not focus on the osteoporosis but rather focus on the recognizable and changeable factors that assisted in its appearance in the first place.
What investigations can be done?
The specifics of the tests needed will depend on the current and past history, but could include the following:
- Blood tests
- Urine tests
- Bone mineral density (DEXA) scans
- MRI
What happens after the investigations?
Once we can recognize the key factors involved in the body’s dis-equilibrium we can then be guided from the results as to how to support a return to equilibrium. Typically the main areas involve:
Diet – eliminate factors which cause gut dysbiosis. Encourage factors that promote good gut function.
Vitamins and Mineral supplementation – to deal with vitamin and mineral deficiencies – this would be either through diet, oral or intravenous supplementation depending on severity.
Environment – eliminate factors that either harm the gut or cause inflammation
Infection – treat any chronic infections
Detoxification – eliminate toxins through diet, supplements or intravenously (vitamins), foot spas, infrared and heat saunas.
Immune support – improve immune function through diet, supplement or intravenous vitamins depending on severity.
How many sessions might be needed?
It may be possible to perform some of the investigations prior to the first consultation. For this to happen I would need to have information about the condition and past history.
The first consultation would then be to go over the results from the tests and to define a plan. From here, typically a review is needed initially at 6 weeks to assess progress and change the program if necessary. From there, the follow up appointments would depend on progress. A repeat of the bone turnover blood and urine test is often needed at some stage between 3 and 6 months after the initial test.
The bone mineral density tests can be repeated at 6-24 months intervals. Other tests may need to be repeated depending on what is found at the initial test.
What can be done now to start helping to restore healthy bones?
A good place to start is to read my booklet Building Blocks for Health. This will explain some simple things you can begin to do that will reduce chronic inflammation and improve immunity.
Think about trying my specially formulated Pre and Probiotic blend of nutrients. More information here.
More information about the tests
Blood and urine tests will help to identify some of the important factors that determine inflammation and bone health.
Standard blood tests include a full blood count, kidney and liver function tests. These are standard tests that you might also get from your GP.
Blood tests looking for markers of inflammation include specific inflammation markers such as ESR and CRP but also indirect markers of inflammation such as Triglyceride. These can also be requested by your GP.
Vitamin D3 is also an important marker of inflammation although this factor is not well known.
The urine organic acids (OAT) test looks at urine metabolites. This test will give a good overall picture of gut microbial balance as well as body and brain nutrient status.
Urine toxicology tests (3 separate tests) will give an idea of toxins from metals and non-metals as well as toxins from fungal exposure called mycotoxins.
Multiple infections blood tests are necessary if there is an indication that the immune system has been compromised for some time and has allowed entry to several viruses or bacteria.
Immunity can be chronically suppressed due to chronic inflammation and low grade infections. The degree of suppression can be measured with specialised blood tests.
Bone Density (DEXA) Scans
The standard imaging test to diagnose osteoporosis is the bone density or DEXA scan. After the initial diagnosis, once treatment has started, a follow up scan will be required to determine if the treatment is working. It may take up to a year before changes are seen on the DEXA scan.
In the meantime, urine tests are also available (Urine NTX) which can serve as indirect markers of bone turnover. These can be done in between bone density scans and also help to refine treatments.
DEXA scans at Oryon Imaging
Oryon Imaging offers DEXA scans to assess osteoporosis for only £115. Visit our DEXA section for more information, or call us on 020 7042 1888 and speak to our friendly team.
Dr Ese Stacey
Dr Ese Stacey practices in Brighton and London. She can be found on either of her websites:
Share this article
Most Recent
Posted on Thu Jul 3, 2025
How Long Does A Shoulder MRI Take?
Posted on Thu Jul 3, 2025
Posted on Tue Jul 1, 2025
Stay up to date
If you’re interested in keeping up with what we’re doing, just leave your email address here and we’ll send you periodic newsletters and other updates.