Sciatica - Spine Health:
The multimodal approach to dealing with sciatica
Sciatica – Spine Health
Posted on Mon Nov 29, 2021
“Sciatica is one of the most common, yet misunderstood, types of pain. As many as 40% of people will get it during their life, and it becomes more frequent as you age.” (Harvard Health Publishing, Harvard Medical School)
We recently sat down with Dr Manojit Sinha, a Consultant in Pain Medicine and Spinal Intervention to explore the topic of sciatica, its primary symptoms, how it is diagnosed and how and when spinal intervention is introduced to help alleviate the symptoms.

Manojit Sinha will be a guest speaker at our Oryon Develop event: Face-to-face: 2nd Essex Pain Symposium: Saturday 29th January
What is Sciatica?
Sciatica is also known as radicular pain; we also call it radiculopathy. Depending on where it occurs in the spine, radiculopathy can have different symptoms and names.
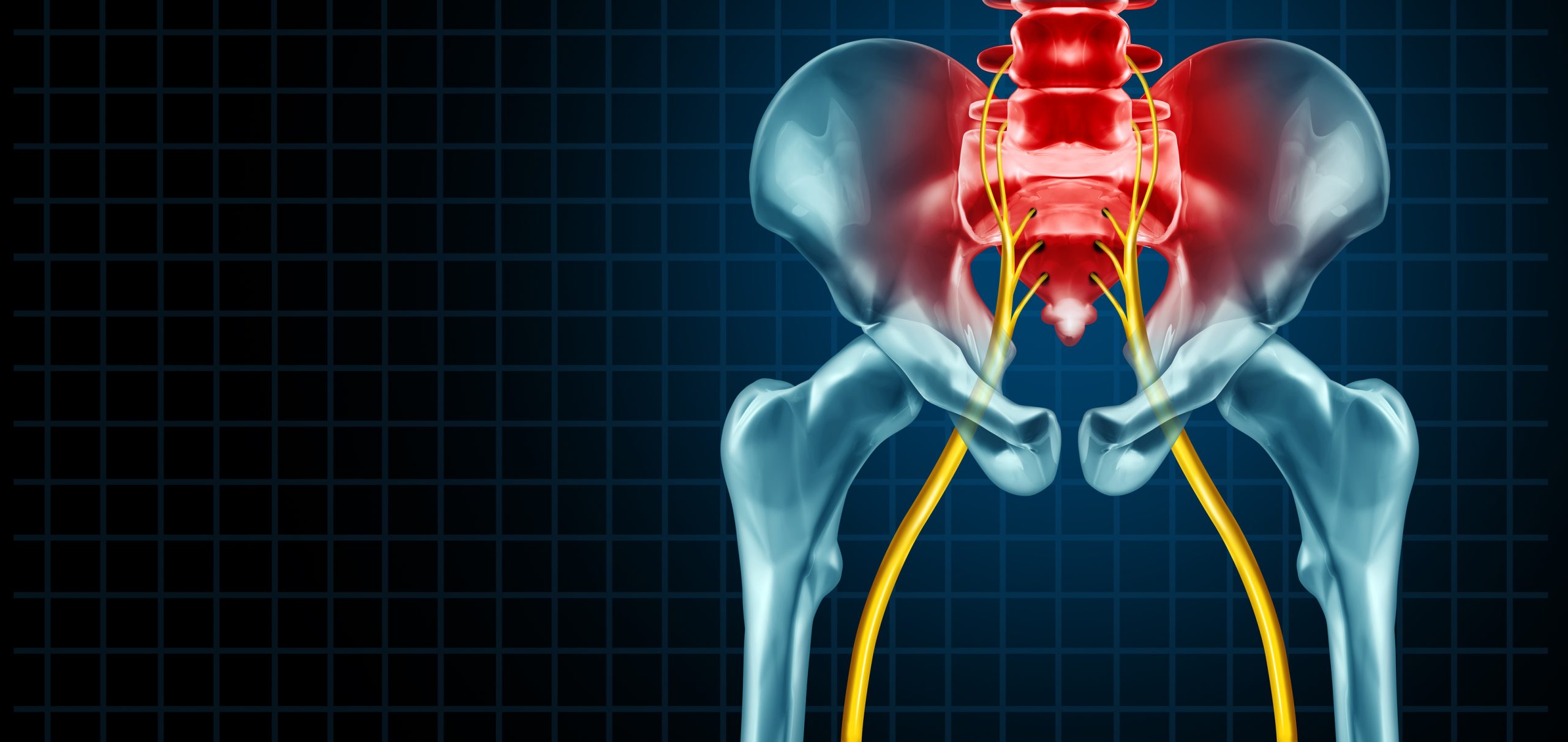
Sciatica is made up of the nerve roots that come from the spinal cord and are mainly caused by irritation impingement or pinching of the nerve roots. Sometimes, it also causes compression.
These are the nerve roots that make up the sciatic nerve, which run from our lower back and around the buttocks area, going down the back of our legs in our thighs and divided into two different nerves, which then supply the foot.
That is why we call it sciatica, but there is no problem in the sciatic nerve itself. The problem is in the nerve root, which constitutes that nerve. Sciatica is not the nerve, but the spinal nerve root, which causes problems there. And this happens due to various reasons.
One of the most common reasons is herniated disc/ slipped disc /prolapsed disc – this is the commonest cause of sciatica, where it can cause pinching irritation or compression of the nerve.
What are the symptoms of sciatica, and how is it diagnosed?
The symptoms can range from; sharp pain, stabbing pain, shooting pain going down the legs with pins and needles and it can sometimes cause a burning sensation. These are all the nerve-related pain and the main symptoms of sciatica. However, occasionally patients can be presented with back pain associated with leg pain; sometimes, they say that I cannot move my leg, my leg goes numb, or it becomes cold. Sometimes they feel hot, so that can vary quite a bit. Also, because the nerves are involved, it means a lot of muscles are also involved. So, you will get aching pain also, but most of the pain is nerve-related.

Is there anything that can be misdiagnosed as sciatica?
There are other conditions, such as spondylolisthesis, where one vertebra slips out of position and causes problems. Degenerative disc – which is a part of our ageing process. All of us will have degenerative changes in our spine, but not all of us will suffer from pain. Spinal stenosis- which is where there is a narrowing of the tunnel where the nerve comes out. Again, this is mostly due to degenerative changes, where it can cause irritation. These can also cause sciatica-like symptoms.
There are also red flags, for instance, if the patient loses control over their bowels or bladder or cannot feel anything between the front and back passage, called Cauda Equina Syndrome. These are the things you must keep an eye on whenever the patient presents them, particularly for GPs; I think it is very difficult for them to be presented with these types of symptoms suddenly. With the minimal amount of time they have with the patient, things can sometimes be missed.
Is sciatica linked to any other medical conditions?
Sciatica is not directly linked with any of any other medical conditions. Still, one of the causes of sciatica is degeneration of the spinal discs, which happens in some patients who have other comorbidities. This mean where there is presence of other diseases such diabetes- degeneration is much quicker.
Smokers also degenerate much quicker than another person who does not smoke.
Most builders have a lot of slip discs, but does it cause any problems? More often probably not because I would not say slip discs are uncommon- it is quite common. If you take an MRI on most of these patients, it will say there is a slipped disc. The slipped disc itself is not a problem. The problem happens when the disc causes problems with the nerve root, which then flares up as sciatica.
So directly sciatica is not linked to other medical conditions, but indirectly there will be other problems.
Is there any surgical intervention for sciatica, and if so, what are the most modern surgical procedures performed to treat sciatica?
Recently, in May 2021, an extensive, randomised control study was a multicenter study that investigated two different things. One of the things we do when we find that the clinical symptoms correlate with the MRI findings- is a nerve root block, which makes a very logical sense- we block the nerve to see whether it helps. In that study, they wanted to find out the difference between a nerve root block and a surgical microdiscectomy.
So, what happens when a nerve gets irritated, pinched, or compressed and now undergoes a lot of inflammation?
It becomes swollen, in quite simple words, and then it causes symptoms. The nerve root block directly deposits the Corticosteroid or any new steroid, which is again anti-inflammatory, and some local anesthetic to numb the nerves and reduce the swelling of the nerve to help with the symptoms. That is the purpose of the nerve block.
This study was compared with a surgical microdiscectomy. It means they take out a few disc materials with the view that it will reduce the protrusion, and reduce the effect on the nerve root.
They did an excellent study, and this was the first randomised controlled study in this country.
They found no difference between the outcome of the two primary studies. They followed those patients for up to 54 weeks (over a year) and they did not find any difference. The only noticeable difference they found was the amount of money the NHS spends on two different types of procedures – which is quite obvious that any surgical procedure will cost very high.
Is it a common misconception that sciatica must be treated through surgery?
Our whole management is multimodal. It does not involve only the injection- injection is a part of the management; we do start on medications; those medications are directed towards the nerve pain- anti neuropathic medication. Medication, which is then combined with physiotherapy – because improving the core muscle strength is especially important in this case.
Not every patient goes for internal. The intervention is only for a selected group of patients when there is a consistent radiological finding with clinical symptoms.
What does the role of imaging play in relation to sciatica?
MRI is a guide; it is not a diagnosis. It becomes a diagnosis when we combine the clinical symptoms which correlate with the MRI. First off we complete a nerve root block, which is diagnostic, and then a therapeutic injection that gives us a very proper diagnosis. This is because we have seen that getting an accurate diagnosis is very important when in pain.
For the spine, until we think that there is any fracture etc. MRI is the best form of radiological investigation, because we can see the bones, we can see the tissues, we can see the nerve, we can see the canals, everything can be seen in MRI. That can be combined with nerve conduction studies because if you are particularly worried about nerve getting pinched, for example, sciatic nerve, or if the patient is presenting with a lot of numbness in the lower limb- we can do enough conduction studies, which can again, find out whether the source of the pain is coming from the periphery itself or from the spinal.
So yes, nerve conduction studies can, if needed, include MRI. However, if we think that there is a fracture or problems with the bone itself, a CT scan is good. However, the first point of diagnosis is MRI – which is the main thing we do 90% of the time.

Are there any activities that can help relieve sciatica symptoms and are there any other alternative methods that can be done currently to help provide relief for unbearable sciatica?
For many patients with sciatica, if they suffer from four to six weeks, it usually has some impact on their functional mobility and, it’s as common with most patients with chronic pain. When they suffer from chronic pain for a long time, it has some effect on their emotions. When that happens, we involve psychologists for any CBT sessions or acceptance behaviour therapy. Spinal manipulations- chiropractors can also help.
So again, it’s a combination of medication, exercises by a physiotherapist, psychotherapy by a psychologist, spinal manipulation, massages by the chiropractors. Then we could do the injections. Suppose everything has been tried, and the patient does not respond to any of those exercises or injections. In that case, as long the MRI findings are consistent with the clinical symptoms- the patient will go for a surgical microdiscectomy which is the last and definitive treatment for sciatica.
I always suggest to the patient whatever helps you. If a patient benefits from Yoga, carry on with Yoga. If they benefit from Pilates, carry on with Pilates.
One of the most important things is self-pacing activities. It means whenever you start an activity, if you pace yourself, you will know which exercise will help and over the pillar of time, you can increase the activity. But again, the most important thing is not to overdo any activity, because if you overdo these activities at some point, you will be in pain.

Conclusion
All of us will undergo some degenerative changes in our spine. Some of us suffer from much more disabling pain, and over time when it becomes chronic; it affects our emotions, stress, anxiety and causes a lot of depression.
Surgery is an option, but everyone should remember that surgery is irreversible. We cannot revert surgery. Medications can be reversed, physiotherapy, psychotherapy, even injections because the injection is just medications. Everything is reversed because the body will break it down. But once the surgery is done, it is done. That cannot be reversed. So, to conclude, whenever we manage, we need multimodal management, that helps more than when you try to do just one thing.
Manojit Sinha will be a guest speaker at our Oryon Develop event: Face-to-face: 2nd Essex Pain Symposium: Saturday 29th January

Share this article
Most Recent
The Most Common Tennis Injuries
Posted on Mon Jul 14, 2025
Do I Need A Referral For An MRI Scan?
Posted on Mon Jul 14, 2025
Posted on Mon Jul 14, 2025
Stay up to date
If you’re interested in keeping up with what we’re doing, just leave your email address here and we’ll send you periodic newsletters and other updates.




